Retinal Detachment
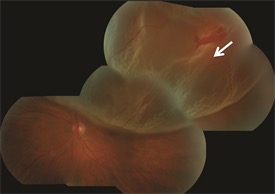
Image of retinal detachment.
Retinal detachment is a separation of the retina from the back of the eye. There are three types of retinal detachments: rhegmatogenous, tractional, and exudative. Rhegmatogenous detachment, the most common form of detachment, is caused by a defect in the retina, either a hole or a tear. Tractional detachment is the result of scar tissue puling on the retina. Exudative detachment is the result of fluid accumulating under the retina. Regardless of the cause, retinal detachment is a serious condition which can lead to permanent loss of vision.
Symptoms of retinal detachment include the acute onset of floaters, light flashes, and a defect in vision. In other cases retinal detachment may develop slowly, but ultimately central vision is involved. Retinal detachment is easily diagnosed by examination of the peripheral retina by a retina specialist. There are multiple treatment options for patients with retinal detachment, including scleral buckle, vitrectomy, and pneumatic retinopexy. Scleral buckling involves placing a silicone rubber band around the eye closing the retinal break. It has a high success rate and a low complication rate. Vitrectomy, sometime combined with scleral buckling, involves removal of the vitreous gel and temporary replacement with a gas bubble. It also has a high surgical success rate. Surgery is performed under local anesthesia as an outpatient. In uncomplicated cases reattachment may be achieved by pneumatic retinopexy, an office procedure involving laser and placement of a gas bubble in the eye. Regardless of the surgical technique, the goal is to achieve the highest rate of success with a single surgical procedure.
Visual results depend on the extent of the retinal detachment, whether the center of vision is involved, and the duration of the detachment. In some case recurrent detachment may occur requiring repeat surgery to remove scar tissue. Ultimately 90% of patients achieve reattachment of the retina with improvement in their vision.